A Body in Motion
15 Jan 2016
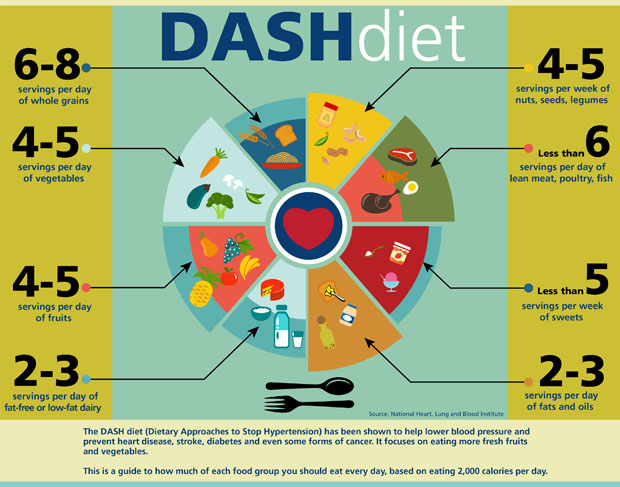
Heart failure is the leading killer of women and men, and we found that the DASH diet remains as one of the most recommended for maintaining a healthy heart, along with exercise five days a week
By SYBIL FIX
From his first in-depth study of the physiology of the body, Dr. Tom Di Salvo became enamored with the heart. He found magic in the seamlessness of its pumping, the effortless beat, the precise regulation of its force.
He first held a beating heart as a medical student, and first observed a heart transplant during his residency. Holding a heart — still beating — in his hand, he said, was nothing less than remarkable. “You feel connected to the force of life,” he said.
The fascination with the heart led Di Salvo to choose a career in cardiology, and understandably so: This fist-sized mechanical pump from which our life stems beats 3 billion times over a lifetime, never stopping from birth to death; it generates its own electrical impulse to run reflexively, and it contains its own molecular chemical factory to keep it working. In its first beat our life begins, and in its last it stops.
“It’s a miraculous gift that only requires feeding and sleeping,” said Di Salvo, who is the newly appointed director of the Medical University of South Carolina’s division of cardiology.
Sadly, though, he said, “It depends on its mechanical parts to work harmoniously together, so if a part is defective, the heart will be inefficient and dysfunctional, and because it cannot renew itself, it will fail and life will end.”
Yet, we continue to treat this vital mechanical part of ours with less care than we treat the motors of our cars, stubbornly ignoring even well-publicized basic guidelines for a healthy heart.
Consider this: Heart disease is the leading cause of death in the United States, and the leading killer of women, claiming more lives than all forms of cancer combined. Heart failure is the leading cause of hospitalization in people over 65. More than one in three women live with some kind of cardiovascular disease. Half of all Americans have at least one risk factor for heart disease, and in the southeastern United States two thirds of adults have high blood pressure. Not surprisingly, a large number of patients with heart failure end up having a heart attack or surgery to prevent one.
The puzzling thing is that more than half of all heart disease is directly attributable to lifestyle: smoking, heavy drinking, eating diets heavy in fat, lack of exercise, lack of preventive care, and lack of treatment for hypertension once it’s developed.
“We were given such a gift, but the reality is that we are quite fragile,” Di Salvo said. Yet, he said, “Most of us spend more time, money, and energy on the upkeep and maintenance of our cars than our hearts.”
The Common Sense
The risk factors leading to cardiovascular disease have been well-described for decades, and the suggested guidelines to counter them have also been well-known for decades. We know what they are: exercise, a healthy diet, no smoking, low cholesterol, moderate drinking, good sleep, and the elimination of nonproductive stress.
A good diet for the heart remains the DASH diet (Dietary Approaches to Stop Hypertension), said Dr. Jason Stroud, a family practitioner for East Cooper Coastal Family Physicians, part of East Cooper Medical Center. It’s an American-style Mediterranean diet, which calls for lots of fruits and vegetables, mostly whole grains, lean meats, fish and poultry, and nuts and beans.
Exercise guidelines vary (see sidebar), but the American College of Sports Medicine suggests that even moderate-intensity cardiorespiratory exercise training 30 minutes five times a week helps maintain a healthy heart, said Stroud.
Di Salvo adds to that list keeping an eye on one’s blood pressure, which measures the pressure in the arteries when the heart beats (the higher number) and when it is at rest (the lower number). He likens high blood pressure to too many heavy trucks traveling on a bridge built for light vehicles. “It is chronic low-stress overload,” he said.
Guidelines newly released by the National Institutes of Health recommend that people who have high blood pressure and one other precondition for heart failure, such as being overweight or having diabetes, lower their systolic blood pressure (the higher number) to no higher than 120. In other words, 120/80 should be the goal for those patients. Generally, patients whose blood pressure is 110/70 are the least likely to have a cardiac incident.
Di Salvo recommends purchasing a pair of heart pressure cuffs. Going back to the car analogy, he said, “You should know your blood pressure like you know how much gas you have in your car.”
All of those healthy heart guidelines continue to be the most important one can follow, said Stroud.
“You hear trendy things all the time,” said Stroud, mentioning recent studies on the benefits of the consumption of coffee, for example. “But we tell patients, you give yourself the best chance by targeting the risk factors we know.”
That’s even truer when it comes to women. Though women may experience the same major coronary artery diseases as men, they are also more likely to develop disease of the smaller blood vessels in the heart, or microvascular disease, said Dr. Pam Morris, associate professor of medicine at MUSC and co-director of Women’s Heart Care, a clinical program for women with heart disease or at-risk for heart disease. This can cause women to have chest pain without evidence of blockages in the major coronary arteries, and microvascular disease may go misdiagnosed and undertreated.
While death rates from heart attack and stroke are declining for both women and men thanks to early detection, the rates of decline are slower in younger women, Morris said.
“It is critical for young women to begin prevention as early as possible. It is never too early to be screened, get blood pressure and cholesterol under control, begin exercising, and maintain a healthy body weight,” she said. “And, tobacco should be avoided at all costs.”
Operating
Once the heart is sick, the chances of surgery are high. The good news is that innovations abound.
Dr. Darren Sidney is an electrophysiologist — an electrician of the heart — with Charleston Heart Specialists, a Trident Medical Center-affiliated practice. Sidney deals with the electrical system that gives the heart its spark. Sidney specializes in finding and fixing irregular heartbeats, also known as arrhythmias, which cause people’s hearts to work too slow, causing fatigue, or too fast, wearing out the system. Among the disorders he treats are atrial fibrillation and supraventricular tachycardia. His patients’ lives are colored by pacemakers that keep the beat up and ablations that keep the beat down. The procedures he performs aim to restore some part of the electrical circuitry of the heart that has gone bad, like removing or fixing the malfunctioning Christmas light that throws off an entire string of lights —but on a cellular level.
Sidney’s is a world teeming with innovations and ever focused on making fixes to the heart in the most precise and least invasive way possible.
“It’s one of the most quickly evolving fields in medicine, constantly changing,” Sidney said. “There are new technologies out and coming out to make ablation more reliable and safer. There are devices ... to prevent blood clots without the use of medications. There are leadless pacemakers. There are devices used to constantly monitor hemodynamics to help custom-tailor therapy for heart failure. It’s one of the most exciting fields in medicine.”
For example, there are new valves that can be inserted non-invasively in patients with aortic stenosis — the narrowing of the aortic valve opening, a critical and widespread malady — who cannot be operated. In the future there will be catheter-based percutaneous approaches to all common cardiac disease affecting the heart valves, Di Salvo said.
While cardiac surgery innovations matter a great deal in saving lives, said Sidney, “Most of what I do is dealing with people with unhealthy hearts ... and a lot of these are things that people can control. Diet, exercise and lifestyle are way more important than what I do.”
Genes
And then there are the exceptions —those who smoke and drink whose heart ticks to 90 without skipping a beat, and, conversely, the people who keel over of a heart attack even though they are fit and don’t smoke. The Jim Fixx’s of the world, said Di Salvo, mentioning the famous runner who died of a heart attack.
That, as they say, is all in the genes, and gene-based precision medicine is where cardiology is headed, together with the rest of medicine, said Di Salvo.
Studies by the National Heart and Long Blood Institute of the National Institutes of Health are moving toward the study of the genes of large groups of people in the context of a databank of millions of genetic variations and combinations, and of individual environmental conditions and lifestyle choices. This will allow doctors to target treatment very specifically to an individual in relation to his or her environment and lifestyle and predisposition to heart disease.
MUSC, meanwhile, is setting up the infrastructure to create a nationally prominent cardiac genetic databank that will help identify people at risk of inheritable cardiovascular disease, said Di Salvo, who was involved in a similar feat at Vanderbilt University in Nashville. The program will comprise data repositories, samples, experts, and genetic counselors.
Already there are FDA-approved genetic tests to determine a risk factor score for certain individual heart conditions due to the variation of one specific gene from one parent. This information can help assess how a certain limited number of conditions might evolve based on past history and help guide lifestyle and treatment decisions. Stroud administers the tests to young patients who experience chest pains but have no risk factors for heart disease, for example.
In the future, however, Di Salvo said genetic study will be able to capture variations in copies of genes derived from both parents, and from various genetic roots and understand how they interact with environment and lifestyle. This will allow doctors to target precise mutations in individuals, as is done currently with some cancers, to tailor medical treatment and to design more precise preventive measures.
“Right now it has been shown that exercise, smoking cessation, dietary changes, stress reduction and the maintenance of a healthy rhythm of life reduce the risk of cardiac disease, but broad therapeutic recommendations do not combat individual risk,” Di Salvo said. “The aim is to tease out the Jim Fixx’s to lower the lifetime risk not only of heart attack but of heart failure that is either genetically determined or a genetically conditioned disease.”
For people with genetic preconditions to heart failure, that is the only salvation. Already certain forms of gene therapy are possible, but eventually, Di Salvo said, it will be possible to edit and replace mutant genes of a defective or sick heart and to affect the way DNA binds and combines to create certain proteins in the heart.
“In the future the hope is that you can add genes or silence two defective genes,” he said. He called this genetic work “a must have.”
In the meantime, for the majority of hearts without genetic misfortune, prevention is still the best bet.
“If you get people to exercise, stop smoking and consuming alcohol in moderation,” said Sidney, “you will have addressed the greater part of the problem.”