Improvements in Diagnosing Cancer
09 Sep 2015
A plethora of new treatments, medicine and detection advancements are helping to slowly win the battle against this leading killer among men and women
By SYBIL FIX
Cancer continues to be one of the most—if not the most—vexing medical problems of our time. It is the second-leading cause of death in the United States after heart disease, and, as mostly a disease of the elderly, it is expected to rise to the number one killer in the next decade. In the near future, up to half of all men and one third of all women are expected to receive a cancer diagnosis in their lifetime. For now, lung cancer remains the deadliest cancer among both sexes, followed by breast cancer for women and prostate cancer for men, then colorectal cancer and pancreatic cancer for both.
Yet, research and advancements in cancer detection, diagnosis and treatment persist doggedly and somewhat heroically: survival rates for most types of cancer are improving, thanks to improvements in cancer screening and treatment, and great strides continue to be made in education and prevention. Hope endures.
“It is a very exciting time. In terms of research, the progress has been immeasurable,” said Dr. Tony Alberg, interim director of the Hollings Cancer Research Center at the Medical University of South Carolina, who has worked with cancer for thirty years. “I cannot imagine a brighter time in terms of diagnosing cancer and being able to provide treatments that are going to prolong people’s lives.”
Cancer refers to a disease characterized by the development and growth of abnormal and uncontrolled cells that multiply and have the ability to infiltrate and destroy normal body tissue, often spreading throughout the body. The simplicity of the definition belies the exceedingly complicated nature of the disease, at whose root are groups of cells whose errant behavior can be compared to that of persistently crazed, rogue, unpredictable teenagers. “Cancer cells have found ways to break all the rules that the body has to manage the behavior and growth of healthy cells,” Alberg said.
All in the Genes
Not only is cancer a complicated family of diseases that affects many different organs in the body, but, underneath their common carcinogenic thread, cancers among those organs differ from each other, and even within cancers in the same anatomical area exist various cell mutations and subgroups of mutations. Hence the word vexing. While treatment of heart disease targets the life and wellbeing of one organ—and great progress has been made in that field—the science of cancer overlaps many organs with many genetic mutations that often respond to first-line treatments, then outwit the treatment, change behavior, and trump the treatment altogether, requiring second- and third-line treatments.
Understanding the behavior of the cells is at the heart of the most effective cancer treatments now, including innovative new drugs that attempt to target that behavior and modify it, or to boost the ability of healthy cells to combat the rogue cells’ behavior.
Among the greatest recent breakthroughs cited in cancer treatment are immunotherapies, drugs that modulate the immune system and neutralize the ability of cancer cells to do what they do best, which is block the immune system. These inhibitors, whose names derive from the types of proteins they block and that are approved for treatment for lung cancer and melanoma, are among the most exciting areas of development, said Dr. Steve Akman, medical director of the Roper St. Francis Cancer Center. These immunotherapies attack the rogue cancer cells and target their very specific type of weakness without affecting healthy cells and thus minimize unwanted side-effects that are more common in chemotherapies, said Alberg.
Equally cutting-age and of great promise are drugs called signal transduction inhibitors. “Research has discovered that cancer is a disease in which normal networks of signals that cells receive to grow, move, and so forth are interrupted. The genes that code for those signaling molecules get damaged,” said Akman—by cigarette smoke, or sun, for example—and they don’t turn off as needed. These drugs intervene by blocking the proteins that cause cancer cells to not turn off.
There are also immunotherapies that reintroduce into the body cells that are boosted with antibodies to attack the cancer cells.
At the very fulcrum of these advances is new genomic understanding of the behavior of cancer cells, allowing the identification and study of the behavior and mutation of specific genes. “Cancer is damage to genetic material. Now we can easily sequence the genetic changes and target those changes very specifically,” Akman said.
This allows for all approaches to the disease to be engineered to target specific mutations. In that regard oncology has become what Alberg refers to as “precision medicine” and what he calls the greatest progress overall in the eventual mastering of cancer, from detection to prognosis and the matching of singular treatments. “This new paradigm looks at genetic ways to target treatment to specific genomic variations. It allows you to see the cells that are behaving errantly...and to kill those cells without adverse effects on other cells,” he said.
The targeting of treatment—be it immunotherapy or inhibitor pharmaceuticals and even some new vaccines—has become exact.
“As we identify genetic mutations that are more prevalent, those are good grounds for research into the most appropriate form of immunotherapy, for example,” Alberg said—a kind of custom-matching of cell mutation to cure. “This is really a new phase—the hope that for more types of cancer and more types of mutations there will be efficacious treatments available.”
In addition to drug therapy, innovations in surgery have also helped make treatment more refined. Robotics, for example, allow doctors a much finer visualization of a tumor, fewer and more exact incisions that decrease pain and recovery time, and greater chances of accomplishing a successful surgery.
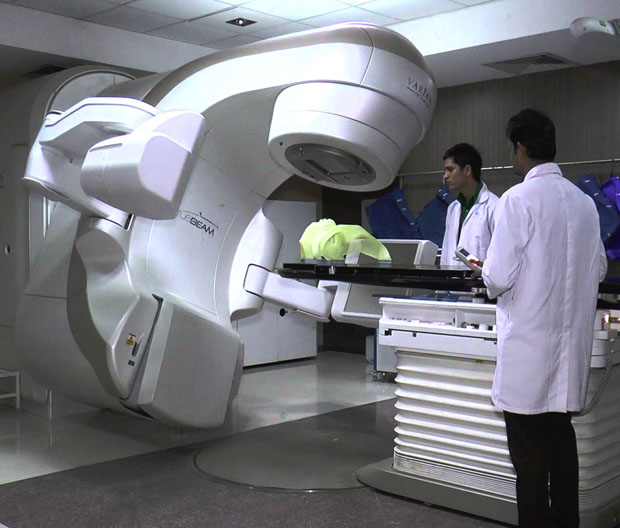
“It is a much more accurate way of doing surgery by increasing the steadiness of the surgeon’s hand and eliminating the human imperfections,” said Ryan Clements, director of Trident Cancer Center. In 2014 the center underwent a $6 million renovation and expansion project, part of whose goal was to incorporate technology that would allow chemotherapy infusion and radiation treatment in one location for greater continuity and efficiency of care. Trident also adopted a more linear, cross-disciplinary team approach to patient management and treatment to make care more seamless and integrated, and switched to a single-vendor system in cancer treatment technology—a bit like switching all of our personal technology to Apple—to decrease redundancy and increase efficiency.
Alongside the renovation came the purchase of new linear accelerators—among them a Truebeam Linear Accelerator—that deliver higher doses of radiation to diseased tissue with sub-millimeter accuracy without affecting surrounding healthy tissue. That kind of finely tuned treatment is emblematic of the greater cell-driven precision that marks cancer treatment today, said Clements.
There are additional innovations in treatment as well. At Roper, for example, said Akman, there are steady innovations in angio-genesis inhibiting drugs—which prevent cancer cells from receiving blood supply needed for survival—and in bone marrow transplantation that significantly reduces the rates of rejection of donor cells, hence increasing the treatment’s success rate.
The Earlier the Better
But early detection and diagnosis of cancer, together with prevention and education, continue to hold the greatest promise for increased patient survival rates. Innovations and refinements in scanning technology are expected to greatly lower mortality rates both from breast cancer and lung cancer. New 3D mammography at each of the local cancer centers allows for the detection of much smaller changes in breast tissue with much greater specificity; new low-dose CT spiral or helical scans allow for the detection of lung cancers at the earliest stages with the use of much lower doses of radiation. Also, research at MUSC indicates promising results in tests for the early identification of lung cancer through biomarkers in the blood, said Alberg.
Clearly, these finer and earlier detection methods allow for greater treatment options and higher success rates in curing the cancer: CT lung cancer screenings alone are expected to decrease lung cancer-related deaths by 6,000 a year, said Akman.
“There is tons of funding being pushed toward cancer research and innovative treatments and research in genetics...but early detection is the key to patient survival,” said Clements. “There are better ways to detect cancer early today and ultimately that leads to curing a patient.”
So-called “next generation” genomic sequencing tests, which are the wave of the future, give much more personalized prognostic information and predictive therapy information. “It can direct all sorts of possible treatments and you can understand what pathways you can alter,” Akman said.
Genetic sequencing can have preventative value as well—for the 5 percent to 10 percent of cancers that can be attributed to genetic predisposition. Most prevention, however, comes from lifestyle choices: quit smoking, not drinking too much, staying out of the sun, eating well, and, it is thought, exercise. Smoking accounts for approximately one third of all cancers. The Hollings Cancer Research Center puts great emphasis on smoking cessation programs to address the habit even in patients who are being treated for cancers other than lung cancers and yet continue to smoke. While it seems intuitive that persistent smoking in cancer patients would result in poor survival rates and increased reoccurrence of cancer, smoking cessation has not been specifically targeted thus far in that group of patients. New recent focus on the understanding of addiction and renewed commitment to targeting addiction in individuals holds promise of further reducing tobacco-related cancers, Alberg said.
Hope
It is impossible to predict when science will have mastered the behavior of cancer cells and the understanding of their many alterations and perversions. Yet, said Akman, “the rate of advances is faster than anything I have seen in forty years. I can barely keep up.”
Akman rattles off the many positive signs: Five new drugs targeting advanced kidney cancer have been introduced in the past five years, while there had been none before 2010; there are more than 150 new cancer drugs in the pipeline now, and new inhibitors are in development. Great progress has been made in drugs to cure lymphatic cancer—drugs that somehow stop cells at growth checkpoints and instruct them not to grow. The death rate from breast cancer has been falling 1 percent to 2 percent every year since 1990; scientist expect to cure 80 percent of cases in the near future. For patients with advanced colorectal cancer, life has been extended on average from eight months to 24-26 months.
Are We Winning?
“If the goal is, ‘Am I going to die of cancer?’ the answer is no, we are not. If the question is, ‘Can I live with it? The answer is yes,” Akman said. “We have converted some cancers into chronic diseases that a patient can live with for a long time. Patients can live very high-quality lives for much longer periods of time...and I am certain that the chances of our ability to detect and treat this range of illnesses will continue to improve.”
“There is a tremendous amount of work to be done,” said Alberg, “but we are moving in the right direction.”
Prostate Cancer
Mortality rates for prostate cancer—contrary to liver cancer, say, or melanoma—have been nearly halved since the early 1990s in the United States (and in South Carolina). Incidence rates have dropped drastically, and age-adjusted 5-year survival rates have risen dramatically.
Yet, an estimated 220,800 new cases of prostate cancer will be diagnosed in the United States this year and an estimated 27,540 people will die of it, according to the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. Prostate cancer remains the leading killer of men after heart disease and lung cancer.
Why is this tiny gland the size of a walnut causing such havoc?
“We do not know,” said plainly Dr. George Keogh, a hematologist and medical oncologist with Roper-affiliated Charleston Hematology Oncology Associates. “It’s an epidemic of people getting this disease, just like breast cancer, and we don’t understand why it happens. It is a major, major public health issue.”
As with all cancers now, the understanding of cancer cells and their genetic mutations is integral to the development of treatments that are successful at curing early-stage prostate cancer and prolonging the life of patients with advanced prostate cancer. The thing that makes prostate cancer exceedingly critical to manage is its position and function.
The prostate is a little exocrine gland snuggled at the bottom of the bladder and at the front of the rectum. It is responsible for the secretion of fluids that mix with sperm to give it mobility and prolong the lifespan of spermatozoa. Because of its delicate position near the bladder and the scrotum, treatment of prostate cancer may have life-altering effects on sexual function and bladder control.
“The difficulty is trying to be certain of how best to use our interventions while not over-treating, and this remains a challenge,” Keogh said.
Treatments for prostate cancer vary greatly based on the stage of the cancer, as they do in most cancers, except that the side-effects of treatment can be much more debilitating and, in many cases, lifelong. Each treatment decision involves insurmountable quality-of-life questions.
The biggest breakthroughs, said Keogh, have been in the development of drugs that, on one hand, block the cancer cells’ reception of androgens—testosterone, in this case, which the cells need to survive—and, on the other, inhibit the production of testosterone. While these therapies may halt the cancer, the side-effects, ranging from hot flashes to bone loss and onset of cardio-vascular disease, are severe. “Blocking the androgens is very hard on patients,” Keogh said.
Improvements in the targeting of radiation and the precision of surgery have helped lower the rates of incontinence and loss of sexual function in the treatment of early-stage cancers. Also, radioactive seeds have proven effective in curing early-stage prostate cancer, and often with little or no effect on a man’s continence or erectile function. Some new chemotherapies are proving effective in inhibiting cancer cell division and are promising for earlier-stage cancer as well. For later-stage cases, the quest is one of buying time.
The holy grail of treatments, said Keogh, is immunotherapy—to teach the immune system to kill the cancer cells and keep them at bay. Small numbers of patients are being treated by mixing their white blood cells with an immuno-stimulatory blend of cells and injecting them back into the body. At this point the procedure is prohibitively expensive, and, in late-stage prostate cancer, which often metastasizes to the bones, it buys little time. Trials are being conducted to assess whether, if administered earlier, it yields greater results. “Immunotherapy holds the greatest promise...because of the decrease in side-effects and because intuitively it makes sense for our own bodies to help cure the cancer instead of drugs that are toxic,” Keogh said.
Overall, and long-term, the biggest ray of hope are genetic signature tests, now under development, that assess the genetic mutations of prostate cancer cells, predict how damaging the type of cancer is and help guide the planning of treatment, said Keogh. Effective predictive genetic testing requires the ability to compare the genetic signatures of current patients to those of large numbers of patients who have gone before them and whose outcome is known. “We look at the signature: if no one died of that particular cancer, we do not operate; if they did, we operate,” Keogh said. Unfortunately, those databanks for prostate cancer lag behind those of breast cancer, for example, in part because of the public awareness campaigns that have surrounded breast cancer in recent years. Interestingly, while prostate cancer is tied to matters that are vital to men, and in a field that is largely male-dominated, its study has suffered from male reluctance to openly discuss the delicate upending effects of this disease, he said.
Nonetheless, survival rates for advanced prostate cancer have been prolonged by months and even years, and improvements in treatments are leading to better quality of life. “We are hoping those improvements come faster. They are never fast enough.”
Certainly, mortality figures suggest that early detection is making a large difference—through digital rectal exams and a prostate-specific antigen blood test (the PSA test). The test remains imperfect and controversial: sometimes higher PSA levels are detected even in the absence of cancer, and low PSA levels may disguise a nascent cancer. Nonetheless, men who observe changes in urination, for example, or erectile problems or blood in semen are encouraged to visit a doctor. New tests for the early detection of prostate-related proteins are being sought.
“We cannot report that we have a huge bump up in cures. They are modest improvements and we have a long way to go,” said Keogh. “But it is important to recognize that advances do come and they are real. It’s just that they are never fast enough.”
Skin Cancer
When talking cancer, the largest and most visible organ of the body, our skin, is not to be neglected. Indeed, skin cancer is the most common type of cancer in the United States, with some 5.5 million cases of non-melanoma skin cancer alone diagnosed in 2012. Incidence rates of melanoma, the most serious form of skin cancer, doubled from 1982 to 2011, according to the American Academy of Dermatology. This year an estimated 74,000 new cases of melanoma will be diagnosed, and nearly 10,000 people will die from it—about one American every hour.
“Skin cancer is preventable and very treatable,” said Charleston dermatologist Dr. Marguerite Germain, of Germain Dermatology, “but if you wait too long and it’s metastasized you have very little hope.”
Indeed, it takes Germain but a few minutes to sum up the skinny on skin cancer, and the dividing line in the narrative between happy and tragic, for both squamous cell carcinoma and melanoma. If the cancer is in situ, on the surface of the skin—even melanoma—it gets removed and in most cases it ends there. If it has penetrated the dermis and the cells have migrated to the lymph nodes, there is a moderate to grave risk of death. Survival rates decline rapidly if the cancer has migrated from local to regional to what is called “distant stage.” (The other most common form of skin cancer, basal-cell carcinoma, does not metastasize or kill, though its removal can cause disfigurement.)
And there is not much more to be said. “Things are being studied,” Germain said, and there are treatments for prolonging life, as in most other cancers, “but depending on how deep it is, if it has metastasized, it is much more likely that you will die. There is no cure. It is a devastating disease.”
Germain is loquacious on detection, however, and equally, if not more so, on prevention.
Detecting skin cancer requires a little bit of time, bright light and a good set of mirrors; while all skin cancer is visible in some way, many cancers are as big as a pimple and often are well-hidden behind an ear, on the back or the scalp. “Usually it’s something new, something that grows, sometimes it bleeds, it is non-healing and it itches.” Old moles that are changing and new moles should be watched carefully as should be all skin of people who have already been treated for one melanoma.
Germain recommends yearly skin checks with a dermatologist and regular self-examinations. While friends, husbands or girlfriends are helpful, she said, nothing is quite like our own knowledge of our bodies. Also, people should ask their hair dressers and barbers to check their scalps and their gynecologists to check their genitalia.
Obviously, when it comes to prevention the number one rule is staying out of the sun, not only for one summer but forever; not only out of direct sunlight, but its reflection, coming from a pool or glass; not only on the beach, but while shopping at the farmer’s market on Saturday mornings. Germain recommends seeking the shade, paying attention to UV indexes in summer, and wearing wide-brimmed hats, zinc oxide-based sunscreen, sunglasses, sun-protective clothing, and protection on ears and lips.
“Most skin cancer is not caused by going to the beach, but by incidental sun exposure which is day to day, when you are strolling down King Street,” Germain said. Also, she said, “Sun damage is cumulative. The skin remembers every second you have spent in the sun in your entire lifetime...and through time we lose our ability to fight off skin cancer...so even if you are staying out of the sun now, you could still get skin cancer due to the sun damage you suffered when you were younger.”
While the incidence of some other forms of cancer is decreasing, the incidence of skin cancer is actually increasing, in part because of early detection, but in part because of environmental and lifestyle issues. “Ozone depletion, suntan booths, leisure time spent getting lots of sun...and emphasis on getting a tan,” said Germain. “Societal norms of beauty encourage tanning—look healthier, look prettier, look skinnier.”
People who have spent a lot of time in the sun are more likely to get skin cancer, and people with a family history of skin cancer are more likely to get skin cancer, and more likely still if they have spent a lot of time in the sun. And this sends us back to early detection.
“The difference between skin cancer and other cancers is that you can see skin cancer. It is detectable and preventable, which is beautiful. Skin cancer has that advantage. But,” Germain said, “you have to look.”